Curvilinear Incision on Iliotibial Tract: Our modified Technique in Harvesting Tibial Cancellous Bone Graft
Clinical Implant Dentistry and Related Research, Volume 17, Supplement 1, 2015
Edward Chengchuan KO
柯 政全
Head
Division of Oral and Maxillofacial Surgery
Kaohsiung Medical University
Kaohsiung, Taiwan
Takao, Formosa
Background:
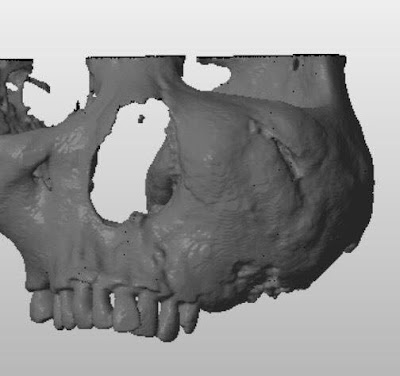
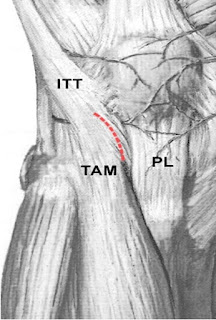
Use of proximal tibia as a donor site has been applied in jawbone reconstruction since the 1990s. Catone and colleagues described a U-shaped incision made on the iliotibial tract during tibial cancellous bone procurement for maxillofacial reconstruction in 1992. We used a curvilinear incision on the iliotibial tract in lateral approach in our tibial
cancellous bone harvesting procedure.
Objectives:
The objectives of this retrospective study are to describe our modified lateral approach for procuring cancellous graft from the proximal tibia and to assess the bone volume, donor site morbidity, and associated complications.
Material and Methods:
Eighty consecutive jawbone reconstructions utilizing autogenous tibial cancellous bone grafts in 78 patients from March 1998 through March 2008 were reviewed. The patient group consisted of 45 males and 33 females, ages 18 to 76 (average age 36.1 1 12.3).Minimal postoperative follow-up period was 3 months. Unlike the traditional U-shaped trapdoor incision on the iliotibial tract, our curvilinear incision was made almost parallel to the fibers of that tract.
Result:
Only mild complications were observed at donor sites, including temporary paresthesia, gait disturbance, and an unpleasant scar. The average procured graft volume was 17.8 mL. We also present the first case of reconstruction of mandibular continuity defects of up to 6 to 7 cm lengthwise by tibial cancellous bone grafting, which has not previously been reported in the English literature.
Conclusion:
The modified incision on the iliotibial tract allowed access to obtain an equally good bone volume from the lateral aspect of the proximal tibia, and it rendered wound closure much easier than the procuring techniques described in the earlier literature.
KEY WORDS: bone graft, Gerdy’s tubercle, iliotibial tract, jaw reconstruction, tibia